Understanding the Causes of Plaque Psoriasis: Uncommon Knowledge
Introduction to Plaque Psoriasis
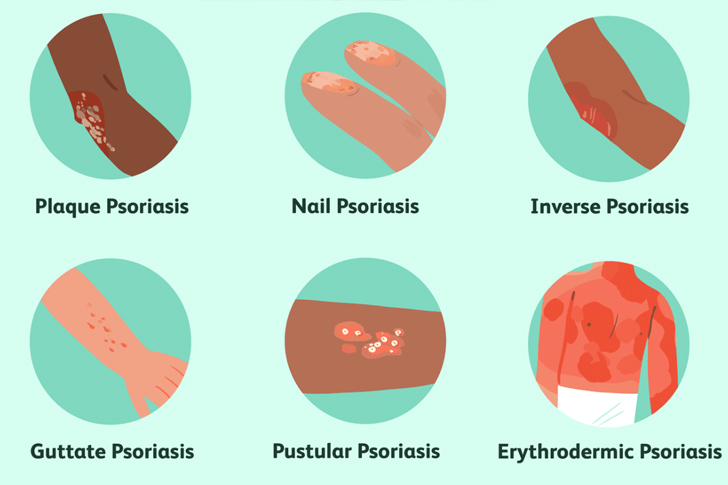
Plaque psoriasis is a chronic autoimmune condition characterized by the rapid buildup of skin cells. This buildup leads to scaling on the skin’s surface. Inflammation and redness around the scales are typical. Often, the scales are whitish-silver and develop in thick, red patches. Sometimes, these patches will crack and bleed. According to the National Psoriasis Foundation, plaque psoriasis is the most common form of psoriasis, affecting about 80% to 90% of people with the condition.
Genetic Factors Involved in Plaque Psoriasis
Research has illustrated that genetics play a crucial role in the development of plaque psoriasis. About 10% of the population inherits one or more of the genes that could lead to psoriasis, but only 2% to 3% of the population develops the disease. The risk increases if one parent has psoriasis and rises further if both parents suffer from it. Scientific studies, such as those from the Human Genome Project, have linked several genetic loci to the predisposition to develop psoriasis, thereby highlighting the multifactorial nature of this condition.
Immune System Dysfunction and Psoriasis
The immune system plays a pivotal role in plaque psoriasis. An overactive immune system causes excessive growth of skin cells, leading to the symptoms of psoriasis. Normally, skin cells grow deep in the skin and slowly rise to the surface. This process usually takes a month. In patients with psoriasis, this production process may occur in just a few days. Because the body can’t shed the skin cells fast enough, they pile up on the surface of the skin, forming plaques. Recent research has pointed to a specific immune cell called a T cell that mistakenly attacks healthy skin cells as if to heal a wound or to fight an infection.
The Role of Inflammatory Chemicals
Underlying immune responses heavily influence the presentation of psoriasis. When the immune system becomes activated, it also triggers the release of various cytokines (immune system proteins), such as tumor necrosis factor-alpha (TNF-alpha), interleukin-12 (IL-12), and interleukin-23 (IL-23). These cytokines can prompt further inflammation and continue the cycle of rapid skin cell production. TNF-alpha, in particular, has been a focal point of psoriasis research and treatment, with several TNF inhibitors being used as effective treatments for reducing plaques and inflammation.
Environmental Triggers of Plaque Psoriasis
While genetics and immune system activity are significant factors, environmental triggers also play a crucial role in the onset and exacerbation of plaque psoriasis. Common triggers include stress, skin injury (such as cuts, scrapes, or surgery), certain medications (including lithium and beta-blockers), and infections (like strep throat). Cold, dry weather can also worsen symptoms. Understanding personal triggers can be a crucial strategy for managing psoriasis outbreaks, as these triggers can vary widely among individuals.
Lifestyle Factors and Psoriasis
Recent studies indicate that lifestyle factors can influence the severity and frequency of flare-ups. Obesity, smoking, and excessive alcohol consumption have all been linked to increased severity of psoriasis symptoms. According to research published in the American Journal of Epidemiology, smokers have almost double the risk of developing psoriasis compared with non-smokers, highlighting the importance of lifestyle choices in managing the condition. Additionally, a nutritious diet rich in anti-inflammatory foods may help alleviate symptoms, although direct links between diet and psoriasis require further study.
Treatment and Management Strategies
While there is no cure for plaque psoriasis, various treatment strategies can help manage symptoms and improve the quality of life for those affected. Topical treatments, such as creams and ointments containing corticosteroids, vitamin D analogues, or retinoids, are frequently used, especially for mild cases. For moderate to severe cases, phototherapy or systemic treatments, which can include oral medications or injectables like biologics, are used. The choice of treatment depends on the severity of the disease, the size of the patches, previous treatment history, and overall health considerations.
Conclusion
Plaque psoriasis remains a complex condition influenced by genetic predisposition, immune system dysfunctions, and various environmental factors. Understanding these factors can help individuals and medical professionals develop more comprehensive treatment plans tailored to the specific needs of each patient. Continued research and personalized healthcare hold the key to better managing this challenging and persistent condition.






Recent Comments