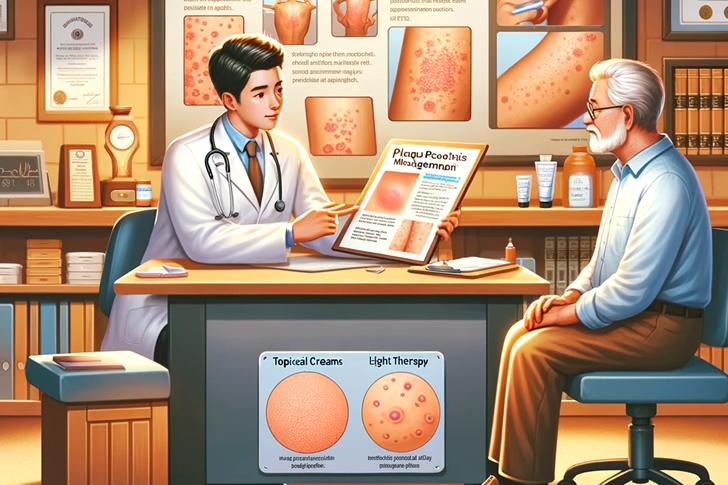
Managing Plaque Psoriasis in Seniors: Essential Insights from Doctors
Plaque psoriasis, a pernynt skin condition, tends to worsen with age, presenting unique challenges for the elderly. It’s crucial for seniors to comprehend the condition’s impact and learn effective management strategies as recommended by healthcare professionals.
Understanding Plaque Psoriasis
Plaque psoriasis is a chronic, uncomfortable autoimmune disease that accelerates the turnover of skin cells, leading to the formation of unsightly red and white scaly patches. These patches are often rough, itchy, and can appear on various parts of the body including the scalp, knees, elbows, and back. In severe cases, it can affect the entire body. Factors such as skin type, lifestyle habits like smoking, obesity, excessive alcohol consumption, and stress can increase the risk of developing this condition.
Early Signals of Plaque Psoriasis
- Red Patches of Skin: One of the first indicators of plaque psoriasis are red, inflamed patches that may appear anywhere on the body. These patches are often covered with silvery-white scales.
- Dry Skin: The affected skin areas can become very dry and may crack and bleed. In some cases, the dryness can be severe enough to cause discomfort or pain.
- Itching and Burning: These symptoms often precede the visible manifestations of the patches. The skin may feel itchy or burn, prompting an initial discomfort that leads to the discovery of the plaques.
- Thickened Nails: Psoriasis can also affect the nails, causing them to thicken, become pitted, or separate from the nail bed, a condition known as onycholysis.
- Scalp Issues: Many people first notice psoriasis symptoms on their scalp, which can appear as scaly, itchy areas similar to dandruff but with a more silvery sheen.
What Does Plaque Psoriasis Look Like?
- Appearance: Thick, red, raised patches (plaques) covered in silvery-white scales.
- Common Areas Affected: Scalp, elbows, knees, lower back, and torso.
- Texture: The patches can be itchy and painful, and in severe cases, the skin at the joints may crack and bleed.
Causes and Risk Factors
- Immune System: Plaque psoriasis is primarily driven by an overactive immune system attacking healthy skin cells.
- Genetics: A family history of psoriasis increases one’s risk.
- Environmental Triggers: Stress, skin injury, certain medications, and infections can trigger or worsen symptoms.
Diagnosis and Treatment Options
Diagnosis typically involves:
- Physical Examination: Visual inspection of the affected skin.
- Medical History: Discussion of family health history and symptom onset.
- Biopsy: Taking a small skin sample to examine under a microscope.
Treatment varies based on severity and includes:
- Topical Treatments: Creams and ointments applied directly to the skin.
- Phototherapy: Exposure to ultraviolet light under medical supervision.
- Systemic Treatments: Oral or injected medications that affect the whole body.
Preventative Measures and Lifestyle Adjustments
- Moisturizing Regularly: Keeping skin moist can help reduce dryness, itching, and irritation.
- Stress Management: Reducing stress through techniques such as yoga, meditation, or therapy.
- Avoiding Triggers: Noting and avoiding personal triggers that exacerbate symptoms.
Psoriasis On Scalp Removal
- Medicated Shampoos: Containing coal tar or salicylic acid, which help reduce scaling.
- Topical Steroids: Effective at reducing inflammation and itchiness.
- Vitamin D Analogues: These can slow down skin cell growth.
Frequently Asked Questions (FAQ)
- What is the main cause of plaque psoriasis?
- It is primarily caused by an overactive immune system that speeds up skin cell growth.
- Can plaque psoriasis be cured?
- There is no cure for plaque psoriasis, but various treatments can help manage symptoms and control flare-ups.
- Is plaque psoriasis contagious?
- No, plaque psoriasis is not contagious. It cannot be spread from person to person.
- How can I prevent psoriasis from getting worse?
- Managing stress, avoiding known triggers, and adhering to treatment plans are key strategies.
Visual Reference Table: Treatment Options
| Treatment Type | Description | Commonly Used Medications |
|---|---|---|
| Topical | Applied directly to the skin | Corticosteroids, Vitamin D analogues |
| Phototherapy | UV light exposure | N/A |
| Systemic | Oral or injected medications | N/A |
Key References for Further Reading
- American Academy of Dermatology: www.aad.org
- National Psoriasis Foundation: www.psoriasis.org
- Mayo Clinic: www.mayoclinic.org
- WebMD: www.webmd.com






Recent Comments